Cervicitis
Content
When to Contact a Medical Professional
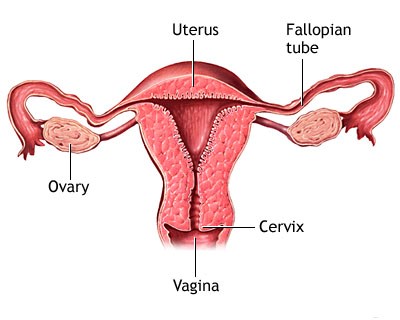
Cervicitis is swelling or inflamed tissue of the end of the uterus (cervix).
Causes
Cervicitis is most often caused by an infection that is caught during sexual activity. Sexually transmitted infections (STIs) that can cause cervicitis include:
-
Chlamydia
-
Gonorrhea
-
Herpes virus (genital herpes)
-
Human papilloma virus (genital warts)
-
Trichomoniasis
Other things that can cause cervicitis include:
-
A device inserted into the pelvic area such as a cervical cap, diaphragm, or pessary
-
Allergy to spermicides used for birth control
-
Allergy to latex in condoms
-
Exposure to a chemical
Cervicitis is very common. It affects more than one half of all women at some point during their adult life. Risks include:
-
High-risk sexual behavior
-
History of STIs
-
Many sexual partners
-
Sex (intercourse) at an early age
-
Sexual partners who have engaged in high-risk sexual behavior or have had an STI
Bacteria (such as staphylococcus and streptococcus) and too much growth of normal bacteria in the vagina (bacterial vaginosis) can also cause cervicitis.
Symptoms
Symptoms include:
-
Abnormal vaginal bleeding that occurs after intercourse, after menopause, or between periods
-
Unusual vaginal discharge that does not go away: discharge may be gray, white or yellow in color
-
Painful sexual intercourse
-
Pain in the vagina
-
Pressure or heaviness in the pelvis
Note: There may be no symptoms. Women who may be at risk for chlamydia should be tested for this infection, even if they do not have symptoms.
Exams and Tests
A pelvic exam is done to look for:
-
Discharge from the cervix
-
Redness of the cervix
-
Swelling (inflammation) of the walls of the vagina
Tests that may be done include:
-
Inspection of the discharge under a microscope (may show candidiasis, trichomoniasis, or bacterial vaginosis)
-
Pap test
-
Tests for gonorrhea or chlamydia
Rarely, colposcopy and biopsy of the cervix is necessary.
Treatment
Antibiotics are used to treat chlamydia or gonorrhea. Drugs called antivirals may be used to treat herpes infections.
Hormonal therapy (with estrogen or progesterone) may be used in women who have reached menopause.
When these treatments have not worked or when cervicitis has been present for a long time, treatment may include:
-
Cryosurgery (freezing)
-
A small probe with an electric current running through it is used to burn or destroy the tissue
-
Laser therapy
Outlook (Prognosis)
Most of the time, simple cervicitis usually heals with treatment if the cause is found and there is a treatment for that cause.
Possible Complications
Cervicitis may last for months to years. Cervicitis may lead to pain with intercourse (dyspareunia).
When to Contact a Medical Professional
Call your health care provider if you have symptoms of cervicitis.
Prevention
Things you can do to reduce your risk of developing cervicitis include:
-
Avoid irritants such as douches and deodorant tampons.
-
Make sure that any foreign objects you insert into your vagina (such as tampons) are properly placed. Be sure to follow instructions on how long to leave it inside, how often to change it, or how often to clean it.
-
Make sure your partner is free of any STI. You and your partner should not have sex with any other people.
-
Use a condom every time you have sex to lower your risk of getting an STI. Condoms are available for both men and women, but are most commonly worn by the man. A condom must be used properly every time.

