Otitis Media – Ear Infection Acute
Contents:
When to Contact a Medical Professional
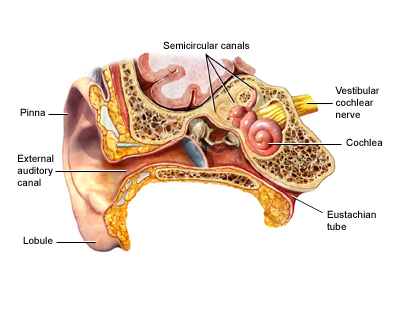
Ear infections are one of the most common reasons parents take their children to the doctor. The most common type of ear infection is called otitis media. It is caused by swelling and infection of the middle ear. The middle ear is located just behind the eardrum.
An acute ear infection starts over a short period of time and is painful. Ear infections that last a long time or come and go are called chronic ear infections.
Causes
The eustachian tube runs from the middle of each ear to the back of the throat. Normally, this tube drains fluid that is made in the middle ear. If this tube becomes blocked, fluid can build up. This can lead to infection.
- Ear infections are common in infants and children, because the eustachian tubes become clogged easily.
- Ear infections may also occur in adults, although they are less common than in children.
Anything that causes the eustachian tubes to become swollen or blocked causes more fluid to build up in the middle ear behind the eardrum. Some causes are:
- Allergies
- Colds and sinus infections
- Excess mucus and saliva produced during teething
- Infected or overgrown adenoids (lymph tissue in the upper part of the throat)
- Tobacco smoke
Ear infections are also more likely in children who spend a lot of time drinking from a sippy cup or bottle while lying on their back. However, getting water in the ears will not cause an acute ear infection, unless the eardrum has a hole in it.
Acute ear infections occur most often in the winter. You cannot catch an ear infection from someone else, but a cold may spread among children and cause some of them to get ear infections.
Risk factors for acute ear infections include:
- Attending day care (especially those with more than 6 children)
- Changes in altitude or climate
- Cold climate
- Exposure to smoke
- Family history of ear infections
- Not being breastfed
- Pacifier use
- Recent ear infection
- Recent illness of any type (because illness lowers the body's resistance to infection)
Symptoms
In infants, often the main sign of an ear infection is acting irritable or crying that cannot be soothed. Many infants and children with an acute ear infection have a fever or trouble sleeping. Tugging on the ear is not always a sign that the child has an ear infection.
Symptoms of an acute ear infection in older children or adults include:
- Ear pain or earache
- Fullness in the ear
- Feeling of general illness
- Vomiting
- Diarrhea
- Hearing loss in the affected ear
The ear infection may start shortly after a cold. Sudden drainage of yellow or green fluid from the ear may mean the eardrum has ruptured.
All acute ear infections involve fluid behind the eardrum. At home, you can use an electronic ear monitor to check for this fluid. You can buy this device at a pharmacy. You still need to see your doctor to confirm an ear infection.
Exams and Tests
The health care provider will look inside the ears using an instrument called an otoscope. This may show:
- Areas of dullness or redness
- Air bubbles or fluid behind the eardrum
- Bloody fluid or pus inside the middle ear
- A hole (perforation) in the eardrum
The health care provider might recommend a hearing test if the person has a history of ear infections.
Treatment
Some ear infections will safely clear up on their own without antibiotics. Often, treating the pain and allowing the body time to heal itself is all that is needed:
- Apply a warm cloth or warm water bottle to the affected ear.
- Use over-the-counter pain relief drops for ears, or ask the doctor about prescription ear drops to relieve pain.
- Take over-the-counter medications for pain or fever, such as ibuprofen or acetaminophen. Do NOT give aspirin to children.
All children younger than 6 months with a fever or symptoms should see the doctor. Children who are older than 6 months may be watched at home if they do NOT have:
- A fever higher than 102°F (38.9°C)
- More severe pain or other symptoms
- Other medical problems
If there is no improvement or if symptoms get worse, schedule an appointment with your health care provider to determine whether antibiotics are needed.
ANTIBIOTICS
A virus or bacteria can cause ear infections. Antibiotics will not help an infection that is caused by a virus. Many health care providers no longer prescribe antibiotics for every ear infection. However, all children younger than 6 months with an ear infection are treated with antibiotics.
Your health care provider is more likely to prescribe antibiotics if your child:
- Is under age 2
- Has a fever
- Appears sick
- Does not improve in 24 to 48 hours
If antibiotics are prescribed, it is important to take them every day and to take all of the medicine. Do NOT stop the medicine when symptoms go away. If the antibiotics do not seem to be working within 48 to 72 hours, contact your doctor. You may need to switch to a different antibiotic.
Side effects of antibiotics may include nausea, vomiting, and diarrhea. Although rare, serious allergic reactions may also occur.
Some children have repeat ear infections that seem to go away between episodes. They may receive a smaller, daily dose of antibiotics to prevent new infections.
SURGERY
If an infection does not go away with the usual medical treatment, or if a child has many ear infections over a short period of time, the doctor may recommend ear tubes.
- A tiny tube is inserted into the eardrum, keeping open a small hole that allows air to get in so fluids can drain more easily.
- Usually the tubes fall out by themselves. Those that don't fall out may be removed in your doctor's office.
If the adenoids are enlarged, removing them with surgery may be considered if ear infections continue to occur. Removing tonsils does not seem to help prevent ear infections.
Outlook (Prognosis)
Most often, an ear infection is a minor problem that gets better. Ear infections can be treated, but may occur again in the future.
Most children will have minor, short-term hearing loss during and right after an ear infection. This is due to fluid in the ear. Fluid can stay behind the eardrums for weeks or even months after the infection has cleared.
Speech or language delay is uncommon, but it may occur in a child who has lasting hearing loss from many, repeated ear infections.
Possible Complications
Rarely, a more serious infection may develop, such as
- Mastoiditis (an infection of the bones around the skull)
- Meningitis (an infection of the brain)
When to Contact a Medical Professional
Call your child's doctor if:
- Pain, fever, or irritability do not improve within 24 to 48 hours
- At the start, the child seems sicker than just an ear infection
- Your child has a high fever or severe pain
- Severe pain suddenly stops -- this may indicate a ruptured eardrum
- Symptoms get worse
- New symptoms appear, especially severe headache, dizziness, swelling around the ear, or twitching of the face muscles
Let the doctor know right away if a child younger than 6 months has a fever, even if no other symptoms are present.
Prevention
You can reduce your child's risk of ear infections with the following practices:
- Wash hands and toys often.
- If possible, choose a day care that has 6 or fewer children. This can reduce your child's chances of getting a cold or other infection, and lead to fewer ear infections.
- Avoid pacifiers.
- Breastfeed -- this makes a child much less prone to ear infections. If you are bottle feeding, hold your infant in an upright, seated position.
- Do not expose your child to secondhand smoke.
- Make sure your child's immunizations are up to date. The pneumococcal vaccine prevents infections from the bacteria that most commonly cause acute ear infections and many respiratory infections.
- Avoid overusing antibiotics. Overusing antibiotics can lead to antibiotic resistance.
Source: http://www.nlm.nih.gov/medlineplus/ency/article/000638.htm

